One of my worries when writing articles about the psychiatric system is that a reader will interpret arguments I make as a form of advice. I want to make clear I am not in the position to make any recommendations. I write from my current experience as a patient and past experience as a physics researcher to hopefully add a few insights where psychiatric research, lived experience and physics meet.
So, when someone seemingly mis-read and mis-interpreted my Lithium Story article, I was a little distressed. I re-read the opening paragraph of my article. While I was telling a story of my opinions at the time, I could see how it might have been possible to interpret it as a recommendation for twice daily dosing. This was not my intention. I am not against once daily dosing.
I realised this was an opportunity to look back and clarify past statements I have made in both my Physics World and Lancet Psychiatry articles.
Physics World Article
I wrote the Physics World article in July 2021. Back then, I was much sicker than I am now1 and very angry. Things seemed simple and clear, when in fact they were cloudy and complicated.
I don’t think writing emotionally is a bad thing. My anger was valid. The simplicity of language in this article helped to get across the pain I felt during my experience as a psychiatric patient. My frustration helped to express the disparity between the scientific rigour I experienced in physics and the relative guesswork of my treatment. My underlying aim was not to disparage all psychiatric practices, but to make the physics community aware that there are physicists suffering out there in an inefficient psychiatric system, and physics researchers have the ability to help improve the situation.
However, writing in a severe emotional state coupled with large gaps in my knowledge about psychiatric research meant that my writing was significantly influenced 2 by what the psychologist Daniel Kahneman calls in his book, Thinking fast and Slow, “What You See Is All There Is” (WYSIATI) . I gave a very coherent and simple narrative (“physics = good and psychiatry = bad”) on a complicated reality 3.
Clarification 1.1: Poor phrasing
While I hope to have pointed out problems in psychiatry that physicists can help with, there are sections in the article where my WYSIATI brain had full control. I have already clarified in this blog my views on counselling, the reason I did not write about the antidepressant Venlafaxine, why I singled out the BRAIN study and my opinion on rating scales. There was, however, one more paragraph in the article I want to clarify:
And yet psychotropic drugs – the main tool psychiatrists seem to use to treat patients – are only given to treat symptoms rather than any underlying psychological traumas. Some psychiatrists I saw even used their assessment of my symptoms to concoct a condition as if out of thin air, before recommending a treatment based on that
From my Physics World article
This was poorly phrased. I imply that I think psychotropic medications only ever treat symptoms. What I meant to say was: unless a quantitative measurement of the brain is taken, psychiatrists and patients are only able to recognise symptoms. I do believe psychotropic drugs can treat underlying causes of conditions, but it is extremely difficult to determine the condition of a patient through symptoms alone.
The previous statement is based on my experience of different psychiatrists diagnosing me with different conditions despite all “seeing” the same symptoms. In my case 4 symptoms were difficult to interpret and did not give a very good indication at the underlying condition. Given my understanding of the nature of complexity, I believe it is possible for two patients displaying the same symptoms to have completely different underlying causes, along with the possibility that two patients with the same underlying causes may present with very different symptoms.
Therefore, trying to prescribe a medication based on fitting a patient’s set of symptoms to an underlying disorder does not seem to be a very useful exercise.
The comment “rather than any underlying psychological trauma” is a strange one. I inadvertently implied that it is possible to characterise psychological traumas as disease states. My actual views on the subject are rather well summarised in an excerpt from the book “The Science of Storytelling” . A colleague of the neuroscientist Leonard Mlodinow explains his view on psychotherapy:
Years of psychotherapy had allowed [me] to construct a helpful story about [my] feelings, motivations and behaviours, “but is it true? Probably not. The real truth lies in structures like my thalamus and hypothalamus, and my amygdala, and I have no conscious access to those no matter how much I introspect” 5
Will storr, The science of storytelling
Clarification 1.2: Why I proposed pregabalin to my psychiatrist
I believe it is unlikely that observation of a patient’s symptoms can help elucidate the disease-causing mechanism(s) within the brain. However, I think that observation of symptom change, after starting a new medication, can give information on whether it “works on” the biological mechanisms of a mental illness.
In the Physics World article, I said that I proposed Pregabalin to my psychiatrist after looking up which medicines the NICE guidelines recommend for GAD. This is not the whole truth.
Around early 2021, I was only interested in proposing disease modifying medications to my psychiatrist. After trialling multiple treatments that at best only brought some symptom relief, it became clear that it would not be enough for me to be enabled to better cope with my symptoms. My condition was too severe. It was essential I found a medication that worked on the core mechanism(s) of my disease.
One of the ways I determined the likelihood that medications were disease modifying was through anecdotes. This might seem strange to hear that a scientist was using anecdotes as evidence to make an informed decision. Well, I wasn’t looking for any old anecdote. I searched for language in the stories of other patients that indicated a clear and obvious effect. In other words, I was searching for a strong “signal”. Most of the anecdotes were not very useful. There were many stories where a patient would say how a certain medication “changed their life” but their descriptions would end up being quite vague. I looked for specific information that indicated a drastic change in the patient’s condition after starting a new medication.
It was comments on a drug rating website that made me suspect that Pregabalin was a potentially disease modifying medication. One in particular sticks in my mind 6. The individual described how they had been in years of therapy for generalised anxiety. They explained that before taking the Pregabalin, they thought therapy was helping quite a bit. They go on to say that after taking the Pregabalin, they realised that the therapy was only helping a little with their generalised anxiety. They said the resulting reduction of their generalised anxiety symptoms was 90 percent due to the Pregabalin, and only 10 percent due to the therapy.
The significant change in the individual’s perception of the severity of their generalised anxiety, 7 along with the specific mention of 90% and 10%, made me think that Pregabalin was disease modifying. I had no way of telling whether I had the same underlying disorder as the individual, but felt it was worth trialling Pregabalin in case I did.
Lithium Story Clarifications
I wrote the Lithium Story because I wanted to make psychiatrists aware of the degree to which the guidelines varied, and the fear that can cause patients. I personally think favourably of lithium – this is despite having had a scary balance issue while on the medication. I have heard of anecdotes where it has transformed the lives of individuals suffering from bipolar disorder. Its effectiveness seems to be backed up by systematic reviews .
Through the following, I hope my intentions will be made clearer.
Clarification 2.1 The “12 hours” was in reference to the standardised serum concentration of lithium, not the elimination half-life
As shown in the graph by Hunter 8 the lithium serum concentration in every patient varies considerably between each dose. I wanted to make sure readers were clear I was referring to blood serum concentration taken at 12 hours and not at any other time on the pharmacokinetic curve. I never referred to a 12-hour half-life.
Clarification 2.2: I did not take lithium for bipolar disorder
I mention briefly in the Lithium Story that rTMS treatment caused my mood to destabilise. I want to elaborate a little here. Immediately after an rTMS session, my mood would lift somewhat dramatically. While I was diagnosed with rTMS induced hypomania, it was questionable whether I actually experienced the condition. The lifting of my mood lasted about two hours, and well, wouldn’t you be a bit over-happy if you finally, finally got a slight break from years of constant misery?
The real problem was what happened after the two-hour lift in mood. Over the following week or so my mental state would fluctuate between severe depression and severe anxiety. The more rTMS treatment sessions I had, the more amplified and longer lasting the swings between anxiety and depression. Nevertheless, the wavelike pattern of my mood always settled back into persistent background generalised anxiety.
I was prescribed lithium as an adjunct to my rTMS therapy. My psychiatrist and I hoped it would even out the fluctuations and prolong the beneficial effect of the rTMS treatment.
On a personal level, I also hoped for some symptom relief. I was aware at the time that lithium had a potential wide range of benefits. As an ion (which are generally “sticky”), I understood it would likely interact with a lot of systems in my body. I found a paper by Robert Post which summarised the potential benefits of lithium .
Given the severity of my condition, any relief was very welcome. I found a blog post published by Young Minds which contained the following anecdote
It’s like living in a goldfish bowl. You can see everything, you can hear everything and everyone can see and hear you, but there’s a difference. You suddenly don’t feel as much. The highs and lows seem to even out, the world isn’t quite so scary. You have protection, a barrier.
Anonymous, What it’s like to take lithium
While not a clear-cut anecdote9, the goldfish bowl description felt compelling to me. Despite experiencing the temporary and strange good mood induced by rTMS, all I really wanted at that time was some relief from the hell that was my generalised anxiety.
A goldfish bowl sounded rather nice.
Clarification 2.3: I felt it was safer to trial lithium over an anti-psychotic medication
Before I found a centre willing to take me on as a private patient for rTMS therapy 10, I was offered an anti-psychotic medication by my local NHS mental health centre.
Regarding the medication, I was given Hobson’s choice: accept what they offered, or I would be left to my own devices. No discussion of how to determine and balance the benefits and risks of the medication. Anecdotally, this seems to be a common occurrence. Such a discussion between me and my past psychiatrists has been rare in my time as a patient.
When looking up information about this particular antipsychotic (as well as antipsychotics in general) used in depression and anxiety, I saw only a small likelihood of a beneficial effect and a much more significant likelihood of an adverse effect, possibly permanent11. So, I declined the offer.
Lithium, on the other hand, seemed likely to provide a beneficial effect. Despite the narrow therapeutic window, I felt that as long as it was managed properly, the medication had only a small chance of producing a significant adverse event. The benefits, in my opinion, outweighed the risks.
Clarification 2.4: I have felt scared every time I have trialled a new treatment
The temporary two hour “lift” in mood directly after my rTMS treatment is not a normal patient experience. Mood improvement is supposed to take weeks.
In all the medications I have trialled so far, weird and unexpected things have happened. It is worth remembering that I had an extreme (and vanishingly rare) reaction to a front-line, normally very safe antidepressant (Sertraline). I was also only four days into taking the introductory dose (50mg). After the severe reaction, my brain was left in a sensitive state. Small changes out of my brain’s neurochemical homeostasis resulted in frightening and often painful symptoms.
Clarification 2.5: I do not have anything against the once-a-day regimen
I started on a once-daily regime, as prescribed by my then psychiatrist. I don’t know why lithium took the “edge” off my severe anxiety so quickly (within the first week). I just know there was a clear and obvious reduction of one particular anxiety symptom in the morning. But, as the day went on, the protective effect slowly wore away before disappearing in the evening. An hour or two after I took the evening dose, the protective effect came back. I slept through most of this benefit.
Once I transitioned to a twice daily dose, a little less of the “edge” was lost, but the protection lasted the entire day. 12 The predominant reason I stayed with a twice daily dosing regimen was because it meant I could take a lower daily effective dose. A common takeaway in some of the articles I was reading at the time was to keep daily lithium dose as low as possible.
To achieve the same reduction of my anxiety symptoms throughout the entire 24 hours with a once daily regimen, I would have likely needed to take considerably more in one dose than I was taking in both my BID doses.
I want to emphasise this is my specific case. The symptom relief was an anxiety reduction effect, not a mood-stabilisation one. I have no general objection to the once-a-day regimen. It just didn’t work as well for me.
Clarification 2.6: I did worry about renal effects
The reasons I felt safer starting on a twice daily dosing regimen were the following:
- On the initiation of lithium therapy, twice daily dosing was recommended by the BNF. Also, while I was not aware of Amdisen’s work at the time, I had read in a 2013 paper by Carter et al. that ”Because lithium serum levels are based on BID dosing, patients should be started on BID dosing to determine an appropriate daily dosage in the therapeutic range, and then switched to SDD” 13
- Kidney disease seemed to be a long-term issue (years). I found a Psychiatric Times article by Chris Aikin, MD which stated that “It takes around 30 years for renal problems to develop in patients taking lithium”. In a paper by Azab et al. the authors mention that “An early stage at which only functional tubulointerstitial damage has occurred may be fully reversible”. Finally, in another Psychiatric Times article by Dr Aiken “High levels of lithium can kill kidney cells, and that may be why one large study found a direct correlation between number of toxic episodes on lithium and renal problems. It also looked like the kidneys were spared in that study if the lithium levels were kept at or below 0.8 [mmol/L]” 14
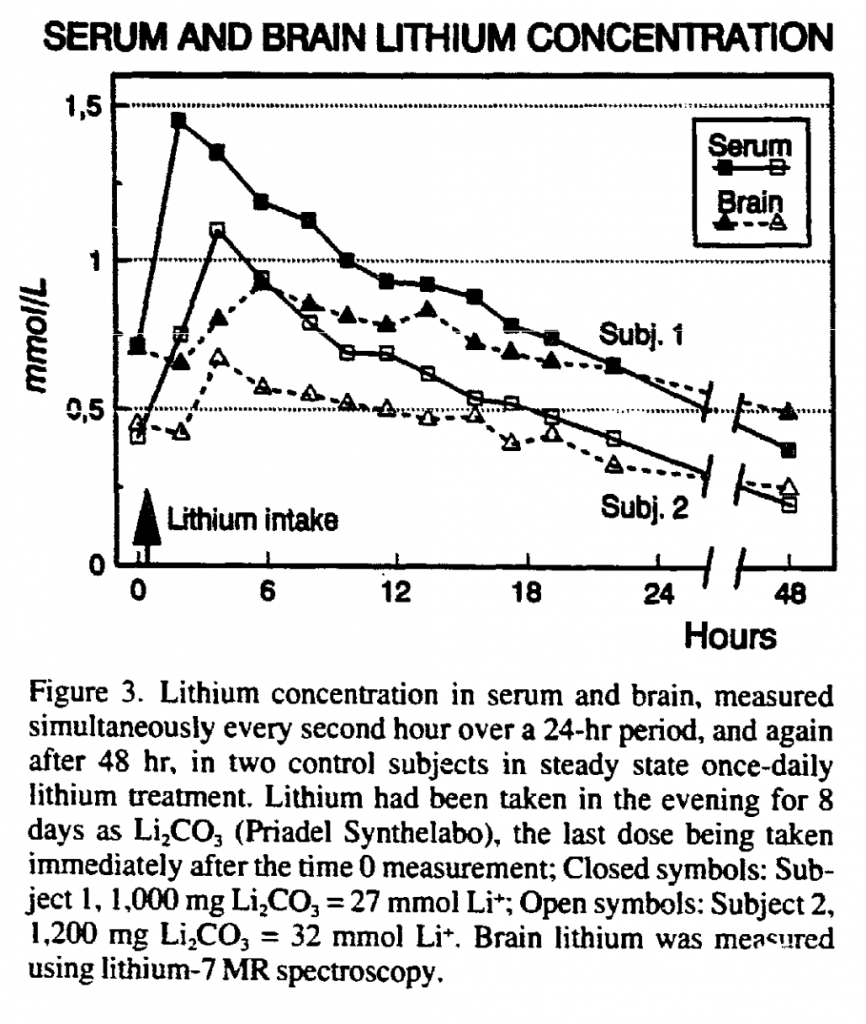
- Acute toxicity seemed to be the main risk in the early stages of starting lithium therapy. I found a graph by Plenge et al. (shown after this list) which seemed to suggest that brain concentration followed serum concentration (with longer half-life in the brain). Splitting the lithium into two equal doses per day decreased the amplitude of the serum pharmacokinetic curve. I reasoned, based on the graph by Plenge et al., that splitting the dose would decrease the amplitude of the brain lithium pharmacokinetic curve too
Long term lithium use was another issue. I decided to remain on the twice daily regimen for the first couple of years. I made my decision based on the academic papers I read, and that gave me some peace of mind, but frankly I feel I have no way of knowing if I made the right decision.
Clarification 2.7: I am no longer taking lithium
Around 6 months after starting lithium, I was prescribed Bupropion. It helped considerably with my depression. At the year and a half mark of taking lithium, I was prescribed Pregabalin, which was the first treatment to reduce my core generalised anxiety symptoms.
However, one of the Pregabalin side effects was an increase in depressive symptoms. I could not go up on the Bupropion as I was already taking the maximum allowed dosage.
Therefore, the decision was made to come off of the lithium very slowly. After coming off of the lithium, my depression symptoms dissipated. So, fortunately, I never had to make the decision about whether to change to a regimen of once daily before bed.
While I am no longer taking it, I found lithium to be a very useful medication. It significantly helped me on my way towards remission.
My main intention when writing the Lithium Story, was to try and help bring awareness to the problems of lithium monitoring guidelines. Lithium has suffered from “bad press” , and I suspect many patients are not offered its benefits . It does have a very narrow therapeutic window, and individuals vary greatly in degrees of tolerance and benefit. To me, this signals the need for prescribers to understand the reasons for the advice on monitoring the blood serum levels, monitoring toxicity signs, and the timing of dosages. Simplified general guidelines are insufficient.
Clarification 2.8: Physics literature example
I mention in the Lithium story that the lithium pharmacokinetic literature does not use the same clarity of language of the physics literature I was used to. But I gave no examples. Therefore, I would like to direct the reader to a recent issue of the journal “Ultramicroscopy”. It is a relatively small journal with an impact factor of 2.2 15
I’ll focus on the open access paper: Quantitative comparison of excitation modes of tuning forks for shear force in probe microscopy .
This paper shows how to conduct a scanning probe microscopy experiment using a quartz tuning fork. Scanning probe microscopes use various “tips” (like the tip of a needle) to determine the surface height of a sample material over a specified area 16. If my understanding is correct, the excitation of a Quartz tuning fork provides height feedback that can be used to help stop the tip from accidentally crashing into the surface of the material, thus damaging both the sample and tip. Through careful analysis, the authors determine the key factors of noise when mechanically or electrically exciting a quartz tuning fork in a scanning probe microscope (more specifically a near-field scanning optical microscope). They then suggest a set up that will produce the optimal signal to noise ratio.
That’s it. There is nothing significantly “new” in this paper. The quartz tuning fork is not used in conjunction with the scanning probe microscope to ascertain any property of any material. While not sexy, I believe this type of paper is one of the most important you see within the physics literature. This paper tells the reader how to properly carry out any scanning probe experiment using a quartz tuning fork. Future researchers will use the knowledge from this paper to ensure their results are of high quality. For more information on why this type of research is important, see Feynman’s lecture on cargo cult science.
The language within the paper is kept as neutral as possible, for example:
Somewhat surprisingly, the authors did not find a published systematic optimization of signal to noise ratios of tuning fork behavior in shear force feedback applications, despite nearly three decades since the introduction of this technique
V.V. Tkachuk et al., Quantitative comparison of excitation modes of tuning forks for shear force in probe microscopy
Translated, the true feelings of the researchers may have resembled: how on earth did no one pick up on this!? Nevertheless, the language remains reserved. The absence of research is not “surprising”, it is “somewhat surprising”.
The authors go to great lengths to be as specific as possible. Processes that influence the results of the experiment, such as cases of background noise, are explained in detail:
The background on the output signal caused by the driving input signal can be removed by cancelling it with a current that has equal amplitude but the opposite phase. This can be implemented by connecting a “dummy load” to the input terminal of the transimpedance amplifier, that is driven with the same frequency and amplitude signal but opposite phase. As this ‘dummy load’ should have no resonance at the resonant frequency of the tuning fork, it is just a capacitor of roughly the same value as the capacitance of the real tuning fork. Precise cancellation of the two currents at the input of the amplifier is done by adjusting the amplitude ratio between the two driving counter-phase signals.
V.V. Tkachuk et al., Quantitative comparison of excitation modes of tuning forks for shear force in probe microscopy
In the places where brevity is desired, plenty of references are given for the interested reader to explore:
The electrodes on the piezo crystal are arranged in such a way that they collect the induced surface charges due to the oscillation in the differential mode and reject the common mode [11], [15], [16].
V.V. Tkachuk et al., Quantitative comparison of excitation modes of tuning forks for shear force in probe microscopy
The amount of detail within the paper allows me, someone who has never worked with a scanning probe microscope, to get a basic understanding of the problem. The graphs are simple and clear. The figure captions concisely and wholly describe the details of the figures. Nothing is left to the imagination (though I will admit the graph legends are a tad confusing). I did not need to go and read three or four other papers to find context. If I wanted to understand the results in more detail, the authors have provided three appendices, and the data for their results is available upon request.
This paper is a good example of the clarity and precision of language expected in physics literature. This does not mean every paper is of the same quality as this one. Standards do vary. As an example, in the same issue of the publication, there is a paper titled: “Cryogenic spectroscopic imaging scanning tunnelling microscope in a water-cooled magnet down to 1.7 K” which contains a clear value judgement statement (a big no-no): “These have achieved sensational research results”. On average, however, I believe the quality of language within physics literature remains high.
I would encourage the reader to compare the paper on quartz tuning forks with some of the pharmacokinetic papers I have referenced in my Lithium Story. I hope you will come to the same conclusion as I did.
Note
I openly welcome criticisms of my work. I am aware I have many blind spots when it comes to my limited knowledge of psychiatry. If it is not too much trouble, I would kindly ask that it be written with my current status as a patient with a mental illness in mind, with correct quotations and references to back up each claim.
References
- I am still very sick
- to a greater degree than normal
- Because of WYSIATI, I try to avoid outright declarative statements. I instead describe my opinions through the phrases like “I believe” and “I think” or through descriptions of events from my perspective.
- and based on the chapter section “the depressing case of psychiatry” in the book “Noise” (see reference [2]), and the left-brain interpreter work by Michael Gazzaniga, probably most other patients
- quote in excerpt from the book “Subliminal” by Leonard Mlodinow (see ref. [4]
- Apologies, I cannot find the original comment to link to
- Without significant change in my symptoms, I am only able to have a relative judgment on their severity. Therefore, when the individual recalibrated their subjective scale for symptoms severity after the Pregabalin, it indicated to me that they experienced an objective and significant reduction in their generalised anxiety symptoms
- included in the Lithium Story Supplementary Material (available online at bottom of article) or my Psychiatry simulations article
- While I did not have bipolar disorder, I was confident that lithium was disease modifying after I read the 2015 New York Times article “I don’t believe in God, but I believe in lithium” by Jaime Lowe. Take a look at the following passage:
By 2000, I had gone seven years without a manic episode. I graduated from the University of California, Davis, with degrees in English and art. I moved to New York and was leading what seemed like a regular life, writing about music for The Village Voice and painting. I went to work every day and paid my rent. If you had met me on the street, I’ll bet you would have thought: This person is normal, has normal problems, approaches the world in a normal way. I decided, along with my psychiatrist of a couple years, Henry Schwartz, to taper off the lithium. Possibly I had been given the wrong diagnosis as an adolescent. Maybe I was past the point of having manic episodes.
After a few months off lithium, I felt energetic, engaged, even electric. It’s hard to know if that feeling was just a ramping up toward mania again or if it was the lifting of a lithium fog. But this is what ended up happening: I turned down jobs and burned all professional bridges with sharp and illogical emails, many of them referring to Eminem; I kept a stash of homemade granola in my pocket to hand out to anyone who would accept a stranger’s dirty pocket granola; I developed an alter ego, a rapper named Jamya; I painted my face with spectacular green-and-gold eye shadow; I was kicked out of a bar without even drinking; I stood on my head every morning; my apartment burned down; I served as the sole witness to a stranger’s wedding on top of the World Trade Center; I wore 800 necklaces and spoke in a slow growl or sometimes a high-pitched squeal; I saved a corgi from being hit by a cab on Central Park West (on which occasion Ben Vereen stopped to call a dog ambulance); I spoke to strangers with the intensity of a car salesman stuck in a Mamet monologue; I preached about Jesus wherever I went, which for a Jew is unusual; I spent almost $700 on butternut squash and assorted seasonal gourds. My clothes smelled of fire, from the burned-out apartment. I scared the scary people on the subway. All that took place over two weeks, maybe three, as I made my way back and forth between Los Angeles and New York.
Jaime Lowe, I don’t believe in god but I believe in lithiumThe specific and clear language describing the drastic change in behaviour gives the indication that the Lithium was doing something significant in the author’s brain.
- therefore before I was offered lithium
- I want to emphasise, I made this decision while very sick and with insufficient knowledge
- Therefore, I went up on the total daily dose slightly and my condition improved further, but this is also when my balance issues started
- Before I read the article by Carter et al. I initially suspected the reason my past psychiatrist called the 12 hour levels “trough levels” was because they were in reference to the 12 hour trough in twice daily dosing. I wondered whether the term was simply colloquialised. After a while, when more and more psychiatrists started to dose once daily, the colloquialisation remained, despite its clearly incorrect usage.
- Dr Aiken recommended once daily dosing in the article and I have not been able to find a source for either the study mentioned or the 0.8 mmol/L claim
- for comparison, the Lancet Psychiatry has an impact factor of 64.3
- the surface of materials, even the ones that look smooth, are actually quite bumpy at small scale. Scanning probe microscopes can give you information about the topology of the material (Like an ordnance survey map of very small areas of materials)
